by Dr. C.V Ramana
What is osteoporosis?
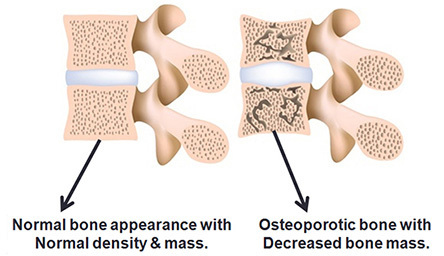
It is the “weakening” or “softening” of bones.
Bone consists of a framework or matrix of collagen and other soft tissue elements. It is then “hardened” by deposition of calcium mineral into the matrix. We think of bone as being a “static” component of the body, but this is not true. Bone is constantly formed and broken down throughout our life as the result of a complex interplay of dueling hormones, health, diet, and activity. In childhood and young adulthood, bone growth is faster than breakdown. People generally reach peak bone mass in their late 20’s. After that, bone breakdown tends to be faster than new bone formation. When calcium is taken out of mature (or fully formed) bone and not replaced, the frame left behind is soft or weak, and easily susceptible to fracture.
Why is calcium needed in the body?
Calcium is an important mineral in the body – it is vital to the formation and strengthening of our bones, but also plays an important role in the function of muscles and nerves as well as innumerable biochemical reactions in the body. Calcium is transported throughout the body dissolved in blood, and so, available to all of our organs and tissues in carrying out their functions. The amount of calcium in the blood is tightly regulated by hormones released into the bloodstream from the thyroid and parathyroid glands (located below the Adam’s Apple), pituitary gland (in the brain), as well as the adrenal glands and kidneys.
Our bones serve as a massive reservoir of calcium that can be tapped when calcium levels in the blood are low due to inadequate dietary intake, inadequate levels of vitamin D in our bodies, or the wrong form of vitamin D due to inadequate exposure to sunlight, or as a result of some medications.
How to know if you have osteoporosis?
Unfortunately, this is a “silent disease” and does not become symptomatic until a bone is fractured, or the back becomes kyphotic (stooped) due to slow collapse of multiple vertebra in the upper spine.
How to find out if you have osteoporosis?
Sometimes the diagnosis may be suggested based on the appearance of bones on x-rays or CT scans that you may have for other reasons. The most reliable way, though, is through a test called DEXA which measures Bone Mineral Density (BMD) in various bones in the body.
Blood tests to determine the level of Calcium, Vitamin D, calcitonin and parathyroid hormone can also be helpful, especially in planning treatment.
Risk factors for developing osteoporosis
Factors that can be modified
* Lifestyle – inactive lifestyle or extended bedrest * Smoking * Alcohol consumption * Inadequate dietary intake * Sex hormones – abnormal absence of menstrual periods or menopause with low estrogen in women, and low testosterone in men * Medications – long term use of steroids, some seizure medications
Factors that cannot be modified
* Sex – women are more prone to develop this than men * Age – bone mass decreases in everyone after the late 20’s * Body size – small boned women are more likely to develop osteoporosis] Ethnicity – Caucasian and Asian women have a higher likelihood, though African American and Hispanic women are also at high risk. * Heredity – people whose parents have osteoporosis have an increased likelihood
How can it be treated?
* Smoking cessation * Decrease alcohol consumption * Lifestyle modification – weight bearing exercises such as walking, jogging, hiking, climbing stairs, playing tennis and dancing are all good. Resistance exercises such as weight lifting or weight training machines are good * Increase dietary intake of calcium and vitamin D * Recommended levels – calcium – more than 1000 mg/day after the age of 30, and 1200 mg/day for women after the age of 50. Vitamin D – more than 600 IU/day for adults up to age 70, and 800 IU/day for men and women beyond the age of 70.
Medications
* Supplemental calcium and Vitamin D * Prescription medications that work in a variety of ways to interfere with the rates of bone formation and breakdown balance * Bisphosphonates (which bind to calcium for deposition in bone) * Estrogen and estrogen analogues * Estrogen receptor modifiers * Calcitonin – hormone * Parathyroid hormone blocker
Who can treat Osteoporosis?
A primary healthcare provider should be contacted for diagnosis and development of a treatment plan. In some cases, they may refer to a specialist for the treatment. Specialists can include endocrinologists, rheumatologists, and women’s health specialists such as an Ob/Gyn.
Dr. C.V Ramana is a vascular and interventional radiologist with more than 20 years of practice experience. He has expertise in all areas of vascular and interventional radiology. Dr. Ramana has a Ph. D from Yale University and MD from CWRU in Cleveland, Ohio where he subsequently completed his fellowship in Vascular and Interventional Radiology at the Cleveland Clinic. https://naadihealthcare.com/ 1 NW 64th Street 73116 Oklahoma City, OK Phone: (405) 608-8884