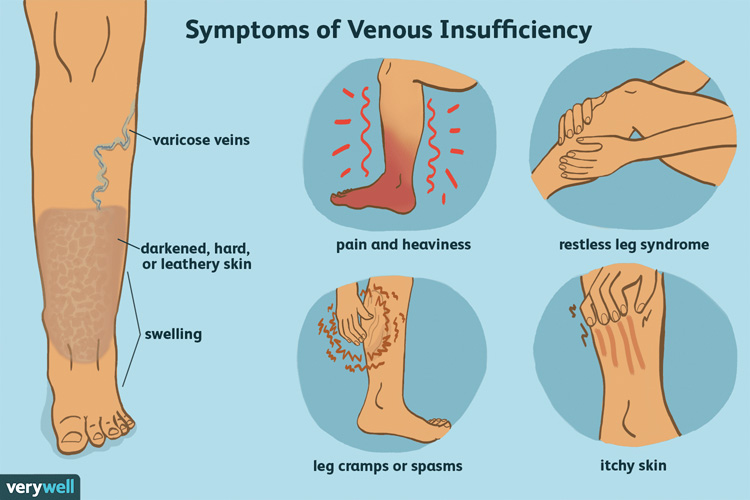
More than 30 million Americans suffer from chronic venous insufficiency, but only 10 percent seek treatment for it, according to the Society for Vascular Medicine. The symptoms of venous disease can vary greatly. Venous symptoms can often be so insidious that, after treatment, patients are surprised to realize how much chronic discomfort they had accepted as “normal”. Common symptoms include burning, swelling, throbbing, cramping, and leg fatigue. Physical examination of the lower extremities is often useful in the diagnosis of venous disease. Some people will notice swelling, changes in the color and texture of the skin, dry scaling, itching skin, visible spider veins or bulging veins in the calf and thigh. Others will experience more serious soft tissue changes that develop as the disease progresses which include chronic inflammation or cellulitis, varicosities that bleed without warning, or wounds that come up like small blisters and take a long time to heal. The most serious complications from chronic venous insufficiency are blood clots and non-healing wounds that become infected – sometimes spreading to bone or into the bloodstream.
Understanding venous disease means understanding the function of the venous system. Veins carry deoxygenated blood back to the heart and lungs to be replenished with oxygen. To reach the heart- blood needs to flow upward, against gravity, from the veins in the legs. The contraction of the muscles in the legs help to squeeze the veins and push the blood upward. Veins contain one way valves to keep the blood flowing up and prevent backflow. Chronic venous insufficiency occurs when these valves become damaged allowing blood to leak backwards and pool in the veins of the lower extremities. Over time, this malfunction of the valves causes weakening of the vein walls. Pressure in the veins and vein wall injury cause a chronic state of inflammation which result in the progressive clinical changes discussed previously, such as swelling, bulging veins, skin changes or the more serious risk factor, blood clots. Blood clots that form in the deep veins of the legs can travel to the lungs and cause serious injury, even death.
My partner has genital herpes while I’m not. I really don’t want to get infected, so take Valtrex for prophylaxis. Although there is no clear evidence of its efficacy for https://smokeypointskin.com/valtrex-online/ this purpose, it’s still better to do at least something than to do nothing. It’s been three months since we are having unprotected sex, and I’m still healthy. So guess that’s the drug that helps.
Risk factors of this condition include:
* Family history of the problem
* Overweight
* Damage to extremity due to injury, surgery, or previous blood clots
* Prolonged sitting or standing
Multiple pregnancies
* Lack of mobility or exercise
In order to diagnose CVI, a complete medical history as well as a physical examination of the patient’s legs are required. A vascular ultrasound may also be useful to examine the blood flow in the legs. Like any disease, CVI is most easily treated in the early stages. Treatment strategies include avoiding long periods of standing and sitting, regular exercise, weight loss, elevation of legs at night, practicing good hygiene and treating active skin infections. Properly fitting, medical grade support hose called compression stockings are a common treatment option from a conservative approach. Compression stockings come in different lengths and compression strength. To ensure a proper fit, compression stockings should be prescribed by a health care provider. Endovenous thermal ablation is a relatively new technique that uses a laser to create heat in the affected vein causing it to collapse. This technique is minimally invasive, can be done in under an hour, involves less pain than traditional therapies such as ligation and stripping, and allows for a quick return to normal activities. Sclerotherapy involves injection of a solution directly into the vein that causes the vein to collapse and disappear.
If you recognize signs or symptoms of CVI, it can be discussed with one of the many specialists who offer treatment options – including cardiologists, vascular surgeons, and interventional radiologists. You are also welcome to call our Vascular Center to discuss the case or make a referral. You can contact us at 405-608-8884.